Veins
What are varicose veins?
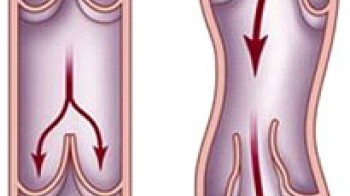
Varicose veins in the legs are veins that have lost their biological function – namely, healthy veins drain blood from the legs towards the heart, thanks to venous valves, or smaller valves in the veins that help venous blood flow against gravity. Varicose veins have damaged valves that have lost their function, resulting in blood retention in the veins of the legs and dilation of the veins (Figure 1). This is an extremely common medical problem, affecting approximately 15% of men and 25% of women.
What are the signs of varicose veins in the legs?
Venous disease of the legs can, in the mildest cases, manifest as small veins that shine through the skin (so-called “capillaries”), then as varicose (sacral) veins in the legs and in the form of swollen legs, and in more severe cases, hardening and darkening of the skin occurs, while in the most severe forms of the disease, wounds form on the skin (“venous ulcers”). Sufferers may not experience any symptoms for a long time, but as the disease progresses, a burning sensation and tingling in the lower legs appear, followed by itching, heaviness in the legs, fatigue, night cramps and restlessness. Venous leg disease can be complicated by the formation of blood clots in the veins, which can potentially lead to life-threatening pulmonary embolism. Bleeding from varicose veins is also possible. Clinical examination usually distinguishes 6 stages of the disease (the so-called CEAP classification):
Stage 1 - telangiectasias (tiny, spider veins, measuring up to 1 mm wide), venules (veins measuring up to 2 mm wide), or reticular veins (measuring up to 4 mm wide) are seen.
Stage 2 - varicose veins (pouch-like) are visible, measuring more than 4 mm in width.
Stage 3 - edema (swollen leg) is visible, but no changes to the skin
Stage 4 - skin changes caused by vein disease are seen (pigmentation, venous eczema, lipodermatosclerosis, i.e. hardening and darkening of the skin).
Stage 5 - changes are visible on the skin, along with an ulcer (wound), which has healed.
Stage 6 - changes on the skin can be seen with the existence of an open ulcer (wound).
If varicose veins do not cause symptoms or are not clearly visible, pay attention to changes in the
color of the skin of the lower legs, darker pigmented skin, the appearance of a capillary network
around the ankles, or a more frequent occurrence of dermatological problems such as eczema...
What causes varicose veins?
The main cause of varicose veins in the legs is genetic predisposition - in the vast majority of sufferers, the occurrence of venous disease in the legs is observed in close relatives. In addition to genetics, the appearance of the disease will also contribute to the lifestyle and habits, such as prolonged standing or sitting, excess weight, multiple pregnancies, taking birth control pills, frequent wearing of high heels and clothing that tightens around the waist. Varicose veins are divided into three main groups: varicose veins, reticular veins, spider veins or telangiectasias. Spider veins are visible on the surface of the skin as red, blue or purple lines. Varicose veins are larger and deeper and often look like bluish protrusions under the skin.
If left untreated,...
Varicose veins are a progressive disease. Spider veins often accompany varicose veins. You may experience pain when standing or walking, along with itching, burning, or tenderness around and in the varicose vein itself, along with swelling of the ankles and feet. Thrombosis, phlebitis, venous ulcers, skin discoloration, lipodermosclerosis, and skin atrophy are also possible. Although spider veins are primarily considered a cosmetic problem, they can cause discomfort such as burning, dull aches, and can progress to varicose veins with all the problems that come with them.
How to treat varicose veins?
Varicose veins are treated by removing the diseased veins from the bloodstream and redirecting venous blood to healthy veins in the legs. Until about ten years ago, this was done by surgically removing the varicose veins from the body. Since this procedure involves multiple incisions and stitches in the skin, most often under general anesthesia, minimally invasive methods of vein treatment have been developed in the 21st century, which are based on closing damaged veins in the body. Vein closure is significantly less aggressive than vein removal and is more effective both aesthetically and functionally.
It is not possible to treat all patients in the same way. One method is better than another in a certain case, but only for that patient or only for a certain type of vein. It is often necessary to combine several techniques in the same patient in order to obtain an adequate, primarily functional, but also aesthetic result.
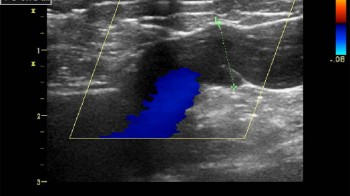
A detailed examination of your veins, which includes a color doppler examination, but sometimes MSCT venography, is crucial for planning the method and sequence of treatment. The introduction of color doppler into everyday phlebological practice is certainly the greatest advance in the diagnosis and treatment of vein diseases. In order to properly treat venous diseases, the source of the reflux must be identified and any contraindication to the treatment must be excluded. Ultrasound is painless and non-invasive. Regular check-ups after the treatment are extremely important, along with later annual check-ups, after the treatment is completed. Dilated sapheno-femoral opening and reflux on the primary valve.
Thanks to our cooperation with eminent experts/ dr.Anton Krnic/Zagreb, Croatia, dr.Karl-Hermann Klein, Burbach, Germany/, top equipment manufacturers/Biolitec, EVRF, Kreussler, Gigaalaser, General Electric/, constant and continuous education in top European centers for the treatment of veins, we are able to offer you a complete and high-quality service in the treatment of vein diseases:
- UGFS treatment-ultrasound-guided injection of foam into diseased veins
- endovenous laser vein ablation (EVLA)
- endovenous radiofrequency vein ablation (EVRF)
- outpatient miniphlebectomy
- minisclerotherapy laser and RFA treatment of capillaries
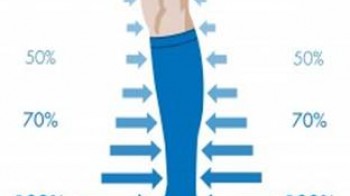
- compression therapy
The most common misconceptions about veins
In the last few years, enormous progress has been made in the understanding of the disease and in the successful treatment of vein disease. This progress was mostly made possible by the routine use of color doppler ultrasound in the diagnosis of vein diseases, as well as progress in laser and radio frequency technology, and many earlier understandings that were considered correct and taken for granted were practically "turned upside down" or turned out to be completely wrong. The most common misconceptions about veins are as follows:
“Women have more vein problems than men.”
Actually, the opposite is true; more studies have shown that men experience varicose veins slightly more often than women, but they are much less likely to seek medical help, even when it comes at the expense of their health.
“Pregnancy causes varicose veins.”
Studies have shown that only women who already have venous reflux (damage to the venous valves) before pregnancy will develop varicose veins during and after pregnancy; in fact, during pregnancy, this condition simply becomes visible or much more pronounced due to hormonal changes in the body and the increased volume of circulating fluid. Women who are pregnant and do not have existing vein problems will not develop them, meaning that pregnancy does not cause varicose veins but can exacerbate or reveal existing issues. On the other hand, even without pregnancy, this problem will manifest sooner or later in life.
A certain number of women (1-2% of the total population) have what is called the congestive pelvic syndrome (pelvic varicosities), and in these women, pregnancy and natural childbirth can indeed be a reason for the appearance of pronounced vaginal and vulvar varicosities as well as varicose veins in the hip and upper thigh regions. If pregnancy caused vein dilations, there would be significantly more women with varicose veins than men, which is not the case, and we would also see a significantly higher incidence of varicose veins in pregnant women, which is also not the case.
“There is no need to hurry to address varicose vein problems.”
This is a common belief even among medical staff today, although it is incorrect for several reasons, primarily because:
- The problem is easier to resolve while it is still small.
- Fewer pathological changes will occur in the skin of the area from which the varicose veins originate.
- A smaller number of veins will be irreversibly damaged and lost the sooner the procedure is performed.
- The procedure is simpler, and recovery is much faster in the earlier stages than in the later stages of the disease.
- Later deterioration (including that which occurs during and after pregnancy) can be prevented.
“Varicose veins are merely a cosmetic defect and can be left as is.”
The bluish or greenish varicose veins that are visible on the surface of the skin are not a problem in themselves but are a sign that the venous pump is not functioning properly; therefore, removing only the visible veins by any means will not solve the underlying problem that led to their appearance. The cause of the venous pump failure must be addressed. A detailed color Doppler examination of the veins and sometimes other tests are necessary to create an appropriate treatment plan and prevent the problem from returning!
“There’s no point in performing interventions for varicose veins since they return.”
Varicose veins have long been considered unimportant or merely a cosmetic issue by both patients and medical staff, and often the diagnosis was made solely based on what can be seen with the naked eye or palpated, and furthermore, surgical procedures were performed based on knowledge gained this way. It is therefore not surprising that there is a high percentage of recurrences of varicose veins following such procedures (according to various studies, 20-25% in the first year post-surgery and up to 75% in 10 years post-surgery).
Only the use of color Doppler has made it possible to see the extent of the problem, potential causes for the appearance of varicose veins, and to plan adequate treatment based on such findings. Properly treated varicose veins should not recur, but it should be noted that some patients may develop new varicose veins due to congenital weaknesses in the vessel walls (the risk is 3-4% per year). Therefore, it is recommended to have an annual follow-up color Doppler examination and to address newly formed varicose veins swiftly while they are still small (usually treated with foam or transcutaneous laser).
“Standing for long periods causes varicose veins.”